Common Diseases of the Spleen
What is the spleen?
The spleen is an intraperitoneal organ. It is located within the abdomen and is the largest organ of the lymphatic system.
What does the spleen do?
The spleen is made up of two different types of tissue which are responsible for mediating its functions, namely:
- The white pulp tissue which is responsible for immune responseas it releases white blood cells (WBCs)in response to any antigen detected.
- The red pulp tissue which works to filter blood by destroying old and non-functional RBCs and recycling the iron components contained in haemoglobin. It also contains WBCs for the destruction of microbes such as bacteria, viruses and fungi,and for signaling to initiate an immune response. It also contains splenic cords which act as a storage area for WBCs and platelets to be released to sites after injury to help aid tissue healing, regulate inflammation, or to compensate after blood loss.
Splenomegaly
What is splenomegaly?
It is the pathologic enlargement of the spleen. A normal spleen is usually less than 12cm in length and weighs less than 200g. Massive splenomegaly occurs when splenic weight is over 1000g.
What are the causes of splenomegaly?
Splenomegaly has a wide variety of causes. The common causes include:
- Haematological: acute and chronic leukemias, hemolyticanemias (thalassemia, RBC defects, sickle cell), polycythemia rubra vera, macroglobulinemia, lymphoma (Hodgkin’s and non-Hodgkin’s), essential thrombocythemia, myelofibrosis
- Tumors and cysts: splenic abscesses, splenic metastases, cysts (hydatid, dermoid), tumors (hemangioma)
- Infections: malaria, schistosomiasis, visceral leishmaniasis (kala-azar), tuberculosis, brucellosis, glandular fever, viral hepatitis, infective endocarditis
- Congestive splenomegaly: diseases that cause dysfunction in splenic blood flow causing backflow of blood into the spleen. Includes liver cirrhosis, Budd-Chiari syndrome, portal or splenic vein obstruction, hepatic vein obstruction, heart failure, hepatic schistosomiasis, constrictive pericarditis.
- Connective tissue disorders: systemic lupus erythematosus, Fealty’s syndrome (triad of rheumatoid arthritis, leukopenia and splenomegaly).
- Other disorders: Gaucher’s disease, Niemann-Pick disease, Histiocytosis X, amyloidosis.
- Massive splenomegaly: chronic myeloid leukemia, myelofibrosis, malaria (hyper-active malarial splenomegaly), leishmaniasis, tropical splenomegaly (idiopathic, Africa, Southeast Asia), Gaucher’s disease
- Splenomegaly in children: infections (glandular fever, cytomegalovirus, viral infections, bacterial, protozoal and fungal infections), autoimmune (juvenile rheumatoid arthritis), haemolysis (hereditary spherocytosis, sickle cell anemia, thalassemia), neoplasia (acute lymphoblastic leukemia, Hodgkin’s and non-Hodgkin’s lymphomas, acute or chronic myeloblastic leukemia, neuroblastoma), inherited disease (Gaucher’s disease and other storage disorders).
Who is at risk of splenomegaly?
Splenomegaly can occur in anyone at any age, but increased risk in;
- Children and young people with infections like mononucleosis.
- Patients with Gaucher’s, Niemann-Pick, and many other inherited metabolic dysfunctions related to the liver and spleen
- People in malaria-prone countries.
What are the signs and symptoms of splenomegaly?
Signs and symptoms differ depending on the cause:
- Mass or pain in the left upper section of the abdomen that can move to the left shoulder in some cases
- Nonacute splenomegaly: Most common type.
- Feeling full after consuming small amounts of food. This is because the stomach is less able to empty because of compression of stomach by enlarged spleen. Chronically leads to unexplained weight loss
- Cytopenia and anemia
- Frequent infections, especially less common infections such as pneumococcus or meningococcus, bleeding, and fatigue.
- Increased bleeding.
- Acute splenomegaly: Sudden onset of pain in the left upper part of the abdomen with tender, enlarged spleen
How to reduce risks of splenomegaly?
Splenomegaly has a wide variety of causes, some of which are hard to reduce the risk of, but in general, the following could help prevent splenomegaly:
- Avoid contact sports and limit activities that could increase the risk of a ruptured spleen.
- It's also important to wear a seat belt. If you're in a car accident, a seat belt can help protect your spleen
How is splenomegaly diagnosed?
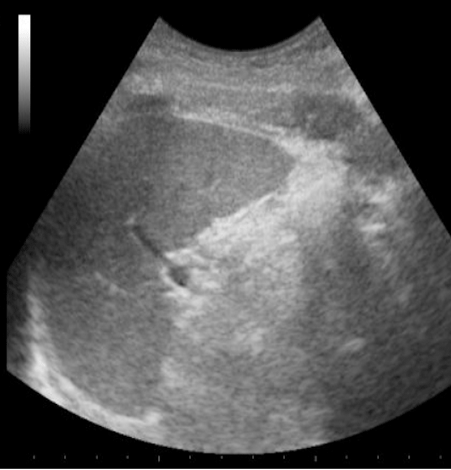
Splenomegaly can be detected on imaging, specifically using ultrasound. Splenic ultrasound is an effective method of determining the size of the spleen, as well as visualizing the impact of spleen size on surrounding organs as this could be the cause of other symptoms being experienced.
It is also important to determine the underlying cause of splenomegaly which can be done using laboratory tests and biopsies.
How is splenomegaly treated?
The management of splenomegaly is dependent on its underlying cause. Some general rules to follow include:
- Ensure full treatment of the cause
- Blood transfusions should be given where necessary.
- Prophylactic vaccinations if there is an impairment in splenic functionality.
- Splenectomy: Can be open or laparoscopic and works well to control or stage disease. Mostly performed as a palliative to give symptomatic relief and has different success rates depending on the underlying cause in question.