Common prostate conditions
Problems with the prostate are common in the population.
Prostatitis: Inflammation of the prostate gland due to a variety of causes including infection. It is the most common prostate problem in men under 50, affecting approximately 10-12% of all men.
General symptoms of prostatitis include:
- Urinary frequency: defined as urination 8 or more times a day due to increased bladder contractions.
- Urinary urgency: the inability to control or hold urine
- Weak or interrupted urine stream with difficulty stopping or starting
- Pain or burn, during or after urination
- Pain in the groin, genital area, lower abdomen, or back.
There are 4 classifications of prostatitis, each with its own more specific set of symptoms, namely:
- Acute bacterial prostatitis: fever, chills, nocturia (frequent urination during sleep), nausea and vomiting, body aches, urinary retention (inability to completely empty the bladder), urinary blockage (total inability to empty bladder), and urinary tract infection (UTI).
- Chronic bacterial prostatitis: nocturia, painful ejaculation, urinary blockage, and UTI.
- Asymptomatic inflammatory prostatitis: no related symptoms. It’s often detected during routine examinations for other conditions
- Chronic prostatitis/pelvic pain syndrome: pain in the central lower abdomen, penis, scrotum, and/or between the scrotum and the anus.
This condition is most common in men with lower urinary tract nerve damage, recurrent lower UTIs, sexually transmitted infections (STIs), HIV or AIDS, use of a urinary catheter, history of other abdominal conditions such as irritable bowel syndrome (IBS).
Treatment of prostatitis is based on classification. Acute presentations are usually treated with up to 4 weeks of painkillers and antibiotics, while chronic presentations require painkillers and antibiotics depending on the length of symptoms, as well as alpha-blockers for those with urination trouble.
Complications of prostatitis include:
- Bacterial infection in bloodstream
- Prostatic abscess: pus-filled cavity in the prostate
- Sexual dysfunction
- Inflammation of nearby organs
- Benign prostatic hyperplasia (BPH): also called benign prostatic hypertrophy. It is increased cell mass leading to the enlargement of the prostate. The causes of BPH are unknown, although links to hormonal changes occurring in men with increasing age have been made.
Symptoms of BPH are related to troubles with urination such as:
- Urinary frequency, urgency, and nocturia
- Hesitancy: problems stopping and starting urination
- Incomplete bladder emptying: continuous feeling of the need to urinate, regardless of frequency of urination
- Straining (Valsalva maneuver): the need to use force to start and complete urination
- Decreased force of urine stream
- Overflow incontinence/Dribbling: due to incomplete bladder emptying, causing small amounts of urine to leak out at a later time.
Treatment for BPH is dependent on the severity of symptoms. Patients with milder symptoms require regular follow-ups and lifestyle changes, but no treatment, whereas patients with more severe symptoms might require medication to decrease prostate size and relax bladder muscles, and surgery if unresponsive to medication.
It is common in men over the age of 50 and is usually not a health concern, except in a few cases where it leads to complications such as:
- Chronic bladder outlet obstruction (BOO): leading to retention,impaired
- kidney function, gross haematuriahematuria, and bladder calculi.
- UTI
- Acute urinary retention: sudden complete inability to urinate
- Prostate cancer: One of the most common cancers in men. It is caused by cells within the gland growing out of control and becoming malignant. There are different types of prostate cancer, including:
- Adenocarcinomas, which are the most common type.
- Small cell carcinomas
- Neuroendocrine tumors (other than small cell carcinomas)
- Transitional cell carcinomas
- Sarcomas .
Symptoms of prostate cancer include:
- Urinary problems such as frequency, urgency, hesitancy, incomplete bladder emptying, pain during urination, and hematuria.
- o Pain in lower back, upper thighs, hips, or chest.
- o Weakness or numbness in lower extremities
- o Unexplained weight loss
- o Fatigue, shortness of breath, or dizziness
- o Rapid heartbeat
- o Paleness of skin
Prostate cancer is mostly a slow-growing cancer, although some do grow and spread quickly. This means treatment of prostate cancer depends on the individual, the type of cancer, and the ability of it to spread.
Prostate cancer is the most common in men of Afro-Caribbean heritage, especially those over 50. Having a high-fat diet or close relatives who have had prostate cancer also increases the risk of being diagnosed with this condition.
Risk factors for developing prostate conditions
General factors that increase an individual’s risk of developing abnormalities in prostate structure and function include:
- Age. Risks for developing prostate abnormalities increase with increasing age, especially in men over the age of 50.
- Race. Men of Afro-Caribbean heritage are more likely to develop prostate conditions, especially prostate cancer, and have double the likelihood of dying from prostate cancer.
- Family history. Men who have first-degree relatives (such as a father, son or, brother) who have been diagnosed with prostate conditions are at increased risk. Also, men who have relatives who have been diagnosed with breast, ovarian or pancreatic cancer are at increased risk of developing prostate cancer due to shared genetic mutations that predispose to the condition.
- Diet. Men with high-fat diets are at increased risk of prostate abnormalities.
- Obesity
- Smoking
- Increased/inflamed prostate size
- History of sexually transmitted infections (STIs)
Ways to decrease risk of prostate conditions
- Dietary changes: Reduce intake of trans and saturated fats and dairy products. Increase intake of fruits and vegetables, especially leafy greens, tomatoes and cruciferous vegetables (such as broccoli and cauliflower).
- Maintain healthy weight: obesity (BMI over 30) is related to increased risk of prostate cancer, hence maintaining a healthy weight will reduce this risk.
- Regular exercise: Sedentary lifestyles and sitting for long periods increase the pressure on the prostate gland and can cause inflammation over time. Aim for 30 minutes of exercise most days as this will help maintain a healthy weight, reduce inflammation and improve immune function.
- Lifestyle changes: Quit smoking and reduce alcohol and caffeine intake as both are linked to increasing prostate risks. Also, be sure to get outside more as increased vitamin D has been shown to protect against prostate diseases
- Maintain good hygiene: Keep the penis and areas around it clean to minimize infections
- Stay sexually active: As men with higher ejaculation rates have lower incidences of prostate cancerbut ensure to practice safe sex to minimize risks of STIs.
Why is early detection for prostate abnormalities necessary?
Screening is essential as it can find tumors before affected patients are symptomatic, therefore allowing for more treatment options where necessary. Screening options also allow for disease monitoring as not all prostate cancers are lifethreatening, and it may be more beneficial to the patient to delay treatments.
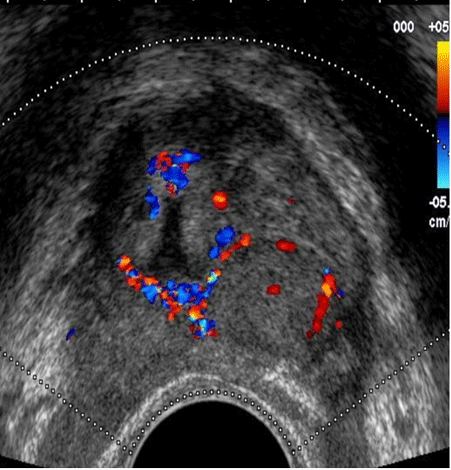
Screening for prostate conditions can be carried out by testing for prostate-specificantigen (PSA) in the blood, however, elevated PSA levels are not specific to any one prostate condition, often requiring follow up diagnostics to determine the cause; there are also risks of false positives(abnormal results when there is no underlying condition), and false negatives (normal results when there is an underlying condition). Transrectal ultrasonography (TRUS) is recommended to determine the size and volume of the prostate gland, as well as any abnormalities. It involves insertion of a transducer into the rectum, next to the prostate to allow for full real-time imaging of the glandand surrounding tissue and does not require general anesthesia. TRUS of the prostate helps to:
- Detect prostate disorders
- Detect enlargement of prostate including BPH
- Detect abnormal growth and masses in the prostate
- Provide guidance during biopsies which is the most reliable way to diagnose prostate cancer.
Who can get screened?
Recommendations for annual prostate screening includes:
- Men aged 50 with average risks for prostate cancer and life expectancy of at least 10 years.
- Men aged 45 with high risks for prostate cancer, especially Afro-Caribbean men with a first-degree relative diagnosed with prostate cancer before age 65
- Men aged 40 with very high risks of prostate cancer, especially men with more than one first-degree relative diagnosed with prostate cancer at an early age.
What are the benefits of screening?
There are many benefits including:
- Detecting cancers early, often before symptoms develop, so they can be easily treated before they spread, hence lowering the risk of morbidity and mortality
- Easily accessible and less expensive
- Does not use radiation or cause any health problems, so it is easy to repeat as often as necessary
- Noninvasive and provides real-time imaging of the gland