Peripheral Artery Disease
Peripheral artery disease (PAD), also called peripheral vascular disease (PVD) is a general body term referring to diseases affecting blood vessels and vasculature outside of the heart and the brain. It is caused by a build-up of substances such as fats, cholesterol, inflammatory cells, proteins and calcium in affected arteries (atherosclerosis) and veins causing them to narrow, or become completely blocked, leading to decreased tissue perfusion in affected areas and limbs. It often lays dormant with most sufferers remaining asymptomatic, until the occurrence of an acute event such as a thrombus, an embolus or trauma causes symptomatic acute ischaemia, an emergency condition requiring immediate intervention and management to prevent loss of limbs and death. This condition most often affects legs, but can also affects the arms, kidneys and stomach. It is estimated that more than 8.5 million Americans, and 200 million people worldwide have PAD, affecting more than 20% of people over 80.
Major complications of undiagnosed peripheral disease:
Despite PAD being a largely silent disease, it has complications that arise as a result of the disease developing over a long period of time. These complications manifest in the form of conditions that affecting many organs within the body, including:
- Coronary heart disease (CHD): The blockages occurring in arteries supplying limbs and organs can also occur in those supplying blood and oxygen to the heart. This reduces perfusion of heart muscles causing damage and leading to CHD such as heart attacks and angina.
- Critical Limb ischaemia: This arises as a result of blood flow to limbs being severely restricted. Symptoms of which include constant burning pain in affected limbs, pale, smooth and shiny skin, muscle wasting and eventually gangrene.
- Renal artery disease or stenosis: This happens when the narrowing or blockage occurs in an artery supplying the kidneys.
- Stroke: A condition which is 3 times more likely in people with PVD. It occurs when blockages occur in arteries that supply the brain leading to ischaemia which is one of the largest causes of strokes.
- Amputation (loss of limb): Often a final consequence of critical limb ischaemia that is not immediately treated. The affected limb becomes gangrenous and needs to be removed to prevent spread of ischaemia to other parts of the body. This most commonly occurs in patients who have diabetes in addition to PAD.
- Poor wound healing: Which occurs due to poor blood supply, oxygen and nutrients, which are required for adequate wound healing, to open wounds and sores. It greatly increases the risks of infections.
- Restricted mobility due to pain or discomfort:One of the major symptoms of PAD is pain in extremities on movement, this can lead to restricted mobility as people affected by PAD are less likely to move to avoid the accompanying pain.
- Severe pain in affected extremity: A result of the ischaemia in the limb caused by restricted flow of blood and oxygen.
Common warning signs of peripheral artery disease
While most patients with peripheral artery disease remain asymptomatic, some display symptoms related to the disease process such as:
- Intermittent claudication which is pain in the buttock, hip, thigh or calf on movement, which disappears on rest.
- Muscle atrophy/wasting or weakness
- Hair loss on legs and feet
- Smooth, shiny skin that is cold to touch
- Brittle, slow growing toenails
- Change in skin colour on legs such as turning pale or blue
- Reduced or absent pulses in feet
- Non-healing, open sores and ulcers on feet
- Erectile dysfunction in men
- Regular movement and exercise: The most effective method of preventing and treating PAD. It is important to remain active to help reduce the risk and severity of PAD and other associated cardiovascular diseases. Simple regimes involving at least 2 hours of exercise a week which are closely monitored and followed can produce results in less than 8 weeks.
- Dietary changes: Reducing the amount of saturated and trans fats, and cholesterol in one’s diet, whilst simultaneously increasing intake of fruit and vegetables can seriously reduce risks of PAD as it reduces the ability of atherosclerosis to occur. It also helps to maintain a weight and BMI within the normal range.
- Smoking cessation: Smoking is one of the biggest risk factors for PAD as smokers have been found to be four time more likely than non-smokers to get the disease, so quitting smoking will help reduce the risk and progression of PAD.
Symptoms of PAD usually develop slowly, over a period, any sudden symptoms that suddenly start or worsen could indicate an emergency requiring immediate medical attention.
Risk factors of peripheral artery disease
The incidence of PAD in any population is influenced by the presence of risk factors common to other cardiovascular conditions which are increasing age, especially in the over 50 age group, positive family history of heart disease, excessive C-reactive protein or homocysteine, diabetes, smoking, high blood pressure, high cholesterol, atherosclerosis, abdominal obesity and kidney disease.
PAD is an incurable condition that often occurs as a result of a combination of cardiovascular risk factors and lifestyle choices, a lot of which can be easily modified to reduce the risk of occurrence, and work to slow disease progression in already affected individuals. This includes:
Typical age of onset
PAD prevalence and incidence increase drastically in age, starting in the over 50 age group, and rising to more than 10% among patients in their 60s and 70s. Due to the overall aging of the global population, it is more likely that PAD will be increasingly common in the future.
Screening for PAD
The rising incidence of PAD in over 50 age groups, combined with ability of the disease to remain dormant until acute life-threatening events happen, it has become more and more important to undergo screening for PAD as this is often the only way the disease is diagnosed, especially in its early stages. Screening for PAD is conducted using the ankle-brachial index (ABI). ABI is a test that compares the blood pressure in the arm with the blood pressure in the ankle. During the test, the two measurements are taken and compared by dividing the systolic ankle pressure by the systolic brachial pressure. In a healthy individual, both blood pressure measurements will be the same or very close making the ABI score 1 or higher. In an individual with PAD, the blood pressure measurement in the ankle will be much lower than the one in the arm due to reduced blood flow making the ABI score less than 1 (any ABI value less then 0.95 is considered abnormal). ABI is also sometimes conducted after physical exertion such as running on a treadmill to help determine the effect, if any, of physical activity on circulation.
Why ultrasound screening?
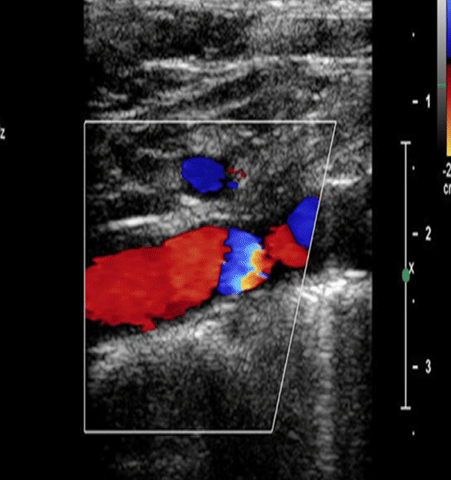
Arterial doppler ultrasound is a more accurate method used to detect PAD. It works by detecting the movement of blood cells and other structures in the body’s circulation, as well as their direction and speed of movement. It allows for the tracking of blood flow in real time which allows for the detection of the exact position of plaques as well as the level of build-up.
How often should you get tested?
Screening is recommended to be conducted annually in adults 65 years or older, adults 50 years or older with risk factors for atherosclerosis or a family history of PAD, and adults younger than 50 years with diabetes and 1 other risk factor for atherosclerosis.