Ultrasound Screening for Deep Vein Thrombosis (DVT)
What is Deep Vein Thrombosis?
When a blood clot forms deep inside one or more veins due to damage to that vein because of injury to the vein during surgery, inflammation or trauma that induces damage to the vein. This partially or completely disrupts the blood flow in the vein, causing pain in the affected body part. It mostly occurs in the extremities, most commonly occurring in the legs.However, it can affect other body parts such as the brain, liver, kidney, and intestines(professional, 2019). The main issue with DVT is that it often does not produce any symptoms, and when symptoms do arise then they may get confused with other health problems and often get diagnosed ultimately when complications of DVT such as pulmonary embolism occur.
What conditions may go underdiagnosed due to DVT?
Although DVT is not fatal, it may become life-threatening when the blot clot in the vein becomes dislodged and travels in the bloodstream to the lungs, where it can disrupt blood flow in the lungs and cause significant damage to the lung tissue, a condition referred to as pulmonary embolism (What is Venous Thromboembolism?, 2020). Pulmonary embolism requires immediate medical intervention to dissolve the clot and can occur without symptoms occurring of DVT.
Another condition that may arise due to DVT is called post-thrombotic syndrome (PTS).It occurs when the valves present in the vein become damaged to due DVT. In severe cases, PTS can lead to permanent disability(What is Venous Thromboembolism?, 2020).
How can I prevent getting DVT?
You can prevent acquiring DVT by(What is Venous Thromboembolism?, 2020):
- Avoiding a sedentary lifestyle, make sure not to sit in the same posture for too long.
- Do not smoke
- After being advised bed rest, try to move around as much as possible, as soon as possible.
- Try to maintainhealthy body weight.
- If you are at risk for DVT or have any blood clotting disease family history then talk to your healthcare provider regarding blood-thinning medications (anticoagulants), and medical compression stockings.
- Opt for loose-fitting clothing.
- When traveling, try to move around or exercise your toes and leg muscles after every 1 to 2 hours.
- Drink plenty of water, as dehydration can cause DVT as well(DVT (deep vein thrombosis), 2019).
How can I reduce my chances of getting DVT?
If you have never had DVT then you can reduce your chances of getting it by getting up and walking every 1 to 2 hours if you are on a long road trip, indulging in physical activity exercises, get moving as soon as possible after being in bed rest, taking blood-thinning medications, and wearing medical compression stockings to reduce your chances of getting blot clot(professional, 2019). However, if you have had DVT, then you can reduce your chances of getting blood clots in the future by making sure that you are taking the medication precisely prescribed by your healthcare provider, and following it up with regular screening and appointments with the doctor to check whether the treatment is working.
What are the symptoms of DVT?
Symptoms of DVT in the leg include (DVT (deep vein thrombosis), 2019) however, you may get them too if the clot is present in the arm or the tummy:
- Swollen veins that are bulging out and are stiff and sore when touched
- Swelling, tenderness, and redness in the affected leg accompanied by warmth
- Cramps and pain, when walking,in the affected leg
Symptoms of pulmonary embolism occurring because of DVT include:
- Trouble in breathing
- Irregular heartbeat
- Lightheadedness accompanied with low blood pressure, fainting spells may occur as well
- Pain or discomfort in the chest which worsens during coughing and breathing deeply
- Coughing up blood
What are the risk factors of DVT?
Although anyone can get DVT, still some factors increase the likelihood of getting it(What is Venous Thromboembolism?, 2020), and they include:
- Increasing age.
- Family history of blood clotting disorders.
- Catheter in the central vein for delivery of medication or for conducting medical tests.
- Taking hormone replacement therapy, birth control pills.
- Pregnancy
- Confinement to bed rest due to injury or surgery.
- Sedentary lifestyle.
- Injury to vein caused by trauma, surgery, or muscle injury.
- Obesity.
- Having had DVT in the past.
- Family history of DVT.
- Having certain chronic medical illnesses such as cardiovascular disease, lung disease, cancer (also chemotherapy), and inflammatory bowel disease.
- Smoking can increase the risk of the formation of blood clots as well(c, 2019).
What are the common methods for treating DVT?
To treat DVT, your healthcare provider will prescribe you blood-thinning medicines such as rivaroxaban, warfarin, etc. that will prevent the formation of blood clots. Usually, this is prescribed for a minimum period of three months, after which they check whether this treatment has worked or not. In the case of the treatment seeming futile, a filter is inserted in the largest vein of the body, the inferior vena cava, to filter any blood clot that may travel towards the heart and lungs, thereby preventing possible health complications.
A newer approach involves breaking down and sucking out the clot from the vein by insertion of a tube in the vein, the patient then is prescribed blood-thinning medicines for some months after undergoing this procedure. In pregnant women, DVT is treated slightly differently(What is Venous Thromboembolism?, 2020). Pregnant women have to be injected with anticoagulant medication throughout the period of their pregnancy and until their baby turns 6 weeks old.
What are the benefits of annual DVT screening ultrasound?
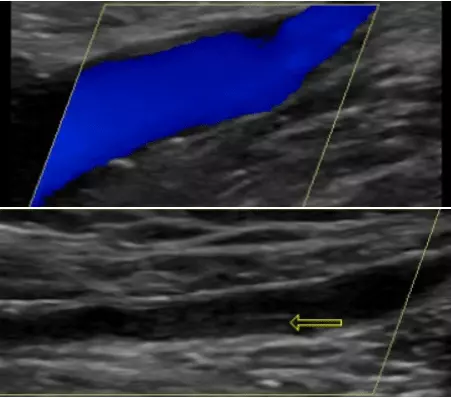
Rest assured that DVT is treatable as well as preventable when it is diagnosed in a timely mannerso that permanent damage to the valves in the vein that will ultimately compromise their function, can be prevented. Ultrasound screening is the least invasive and painless way to get yourself screened for DVT. It gives a clear picture of the blood flow in the veins and identifies whether clots are present in the blood. During the procedure, the technician may apply pressure on the arm or leg to see if the vein is compressing under pressure. If it does not compress then this may indicate the presence of a blood clot(professional, 2019).