Breast cancer
Breast cancer refers to a subtype of tumors arising from the mammary gland in the breast. It is the most common invasive cancer in women, the second most common overall, after skin cancer, with approximately 1 in every 8 women developing breast cancer, and currently the leading cause of cancer deaths in women.
Signs and symptoms of breast cancer
Breast cancer tends to remain asymptomatic in its early stages, with signs and symptoms often appearing in later stages, including:
- The initial presentation is usually as a lump or area of increased tissue density in the area of the breast and/or armpit.
- Pain/soreness in the breast or armpit unrelated to the monthly cycle.
- Pitting/dimpling of the skin which looks like the surface of an orange peel (peaud’orange).
- Changes in skin color such as increased redness
- Presence of a rash (eczema-like) around the nipple area
- Nipple discharge which may contain blood
- Sinking or inversion of the nipple
- Changes in the size and/or shape of the breast and/or nipple.
- Changes in breast or nipple skin such as peeling, flaking, or scaling.
- Swelling of lymph nodes in the neck and/or armpit.
Risk factors for breast cancer
The causes of breast cancer remain unknown, however, the factors that increase the risk of diagnosis are:
- Age : The risk of developing breast cancer increases with increasing age with 8 out of 10 cases occurring in menopausal women after the age of 50.
- Gene mutations : Certain gene mutations have been linked to increased risks of developing breast cancer, namely mutations in the BRCA1, BRCA2, TP53, and CHEK2 genes. Recommendations are in place for individuals with family histories of breast, ovarian, fallopian tube, or peritoneal cancer to get gene testing, especially individuals with Ashkenazi Jewish ancestry.
- Hormone exposure : Early age of menarche and late menopause increases exposure time toestrogenwhich increases risk of breast cancer.
- Reproductive history : Not having children or having children later in life can also slightly increase risk of breast cancer due to uninterrupted estrogen exposure.
- Breast density : There is increased likelihood of breast cancer due to increase in connective and fatty tissue. This can also make diagnosis more difficult as the dense tissue can obscure tumors on imaging.
- Previous breast cancer diagnosis : People who have previously had breast cancer or early non-invasive cancerous cell changes have an increased likelihood of getting it again.
- Previous history of non-cancerous breast diseases : People with certain benign breast lumps or cell changes such as atypical ductal hyperplasia and lobular carcinoma in situ have increased likelihood of developing breast cancer
- Family history of breast and/or ovarian cancer : Having a close relative who has previously had breast or ovarian cancer increases one’s likelihood of developing breast cancer, especially if it is a first-degree relative such as a mother, sister, or daughter.
- Previous history of radiation therapy : People who have previously undergone radiation therapy for previous cancers, especially to the chest area such as for Hodgkin’s lymphoma, have increased risk of developing breast cancer. Certain radiation-based medical procedures such as X-rays and CT scans may also moderately increase breast cancer risk
- Previous usage of diethylstilbestrol (DES) : DES is a medication that was administered to pregnant women in the USA between 1940 and 1971 to reduce miscarriages. It has since been associated with increased rates of breast cancer in both women and their offspring.
- Use of hormonal medication : Taking hormone replacement therapy (HRT) that combines both estrogen and progesterone is linked to increased risk of breast cancer when taken for over a year. Oral contraceptive pills have also been shown to moderately increase the risk of breast cancer. Risks of breast cancer have been shown to decrease once you stop using these medications, returning to baseline after 10 years.
- Race : Women of Afro-Caribbean descent have been shown to have higher rates of breast cancer, with increased likelihood of developing more aggressive forms of breast cancer with resultant increased mortality of 40% when compared to women of Caucasian descent.
- Lifestyle factors : Obesity and alcohol consumption increase the risk of breast cancer. Obesity becomes a greater risk factor after menopause due to an increase in estrogen levels. Risk of breast cancer is also shown to increase with increase in alcohol consumption
Prevention of breast cancer
There is no way to absolutely prevent breast cancer, but things can be done to reduce risk of developing the disease such as:
- Lifestyle modification : Increase in physical activity to maintain a healthy weight and decreasing alcohol consumption reduces risks of breast cancer.
- Reproductive history : Pregnancy and breastfeedingcan reduce risk of breast cancer, as it causes a drop in estrogen exposure.
- Hormone therapy : Taking estrogen-only hormone therapy post-hysterectomy, using selective estrogen receptor modulators or aromatase inhibitors and inactivators.
- Prophylactic mastectomy : This is pre-emptive surgery to remove breasts. It is usually indicated in people at high risk of developing breast cancer such as individuals who test positive for an associated genetic mutation at gene testing and have close relatives who have had breast, ovarian, fallopian tube,or peritoneal cancer.
- Ovarian ablation : Removal of ovaries which can be done surgically, using radiation or medication in an effort to lower or stop estrogen production. Usually only indicated in women at high risk.
- Medication : There are 3 types that can reduce risk of breast cancer and are indicated for women at high risk. Tamoxifen for pre- and post-menopausal women, anastrozole and raloxifene for post-menopausal women.
Breast cancer screening
Breast cancer is sometimes diagnosed after symptoms appear, but many women remain asymptomatic until the cancer has entered a late stage and spread making it harder to treat and increasing the risk of mortality.
Why is breast screening important?
Breast cancer screening is used to detect early-stage cancer. The detection of breast cancer in its early stages increases the chances of successful treatment and reduces the risk of long-term effects on quality of life and death. Since the development of screening programs, the majority of diagnosis has occurred as a result of the screening process which becomes increasingly important as the lifetime risk of breast cancer continues to increase from around 5% in the 1940s to around 12% more recently.
Breast screening guidelines
The guidelines for women at average risk (women with no personal or strong family history of breast cancer or related genetic mutations, women with no history of radiation therapy to the chest area before the age of 30)as recommended by the American Cancer Society (ACS):
- Yearly screeningsaged 40 to 54
- Screening every 2 years aged 55 and older.
Note that this differs from the recommendations of the US Preventive Services Task Force (USPSTF) which are:
- Screening every 2 years from the ages of 50 to 74
- Can be considered for women aged 40 to 49 if benefits outweigh risks
- Women 75 and older should continue screenings if life expectancy is 10 or more years.
Women at higher risk of breast cancer are recommended to start yearly screenings at an earlier age.
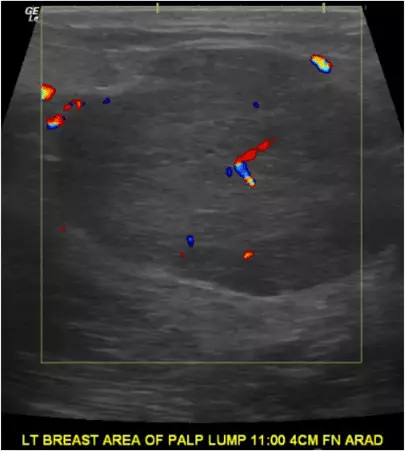
Breast ultrasound
Breast ultrasound is a safe, painless, and non-invasive procedure that uses sound waves to evaluate and diagnose palpable or identifiable lumps or masses.
Benefits of breast ultrasounds
- Ultrasounds can better detect presence of lumps in breasts of higher density
- Can determine if lump is as a result of a malignant solid mass or a benign fluid-filled cyst.
- More sensitive for the detection of invasive cancer in nonfatty breasts
- Can detect breast lesions that would be invisible during physical examination and on other imaging options.
- It is used to guide biopsies if necessary for further diagnosis
- It is safe and painless, requiring no breast compression.
- Your results are read by a Board-Certified Radiologist.
- It does not require a prescription.
- Breast ultrasound takes 15 – 20 minutes on average.
- Breast ultrasound is better for all women, but most especially critical for the 50% of women with dense breast tissue.
Who should get a breast ultrasound?
- Women under the age of 35.
- Women at high risk of breast cancer who cannot undergo an MRI exam
- Women who are pregnant and therefore cannot be exposed to X-rays.
- Women with higher breast density.
- People who require further diagnosis of lumps or masses detected during a mammogram.
What can be seen on the breast ultrasound?
The high-frequency sound waves produced by ultrasound produce images of the inside of the breast to show any lumps or areas of abnormalities. Breast ultrasounds are able to distinguish solid from fluid masses, as fluid appears as the darkest material on a sonogram, and solid lesions may appear a little brighter or a little darker than their surroundings. Solid malignant masses typically appear on ultrasound as nodular structures that are slightly darker than their surroundings and have ill-defined borders.
The ultrasound is interpreted by a board-certified radiologist (a doctor who specializes in imaging modalities).