What are the risk factors for AAA?
Even though it is not certain what causes AAA, here is a list of risk factors(Abdominal aortic aneurysm, 2020) that predisposes people to develop AAA.
- Smoking
- Family history of AAA
- Chronic high blood pressure
- Chronic obstructive pulmonary disorder
- High cholesterol
- Atherosclerosis
- Obesity
- Congenital connective tissue disorder
- 60+ age*
- Male gender
*Although the risk of AAA development increases with age, however, if someone younger suffers from chronic high blood pressure or high cholesterol then they are at risk for AAA development as well.
What is the usual age of onset?
It is usually 50+ for males and 60+ for females(Singh, n.d.).
What are the signs and symptoms of AAA?
In most cases, people are asymptomatic. However, symptoms like persistent severe back pain and persistent severe stomachache may be warning signs of AAA. Some people might feel a constant pulsing sensation near their navel area. While in rare signs such as discoloration in feet and toes, and sores on feet may present themselves because of the accumulation of blood clots in the affected area due to AAA(Singh, n.d.).
What are the warning signs of complications?
The common warning signs include;
- Persistent pain in the stomach and back
- Blood clots that can get stuck in other arteries and cause ischemia in the tissue supplied by that artery.
- Large aneurysms can compress neighboring structures, such as the inferior vena cava which might get compressed,when its function gets compromised (Punwani, 2014).
- Internal bleeding in the abdominal cavity.
Why is screening for AAA necessary?
Abdominal aortic aneurysms are not dangerous if they are small because the risk of rupture is low.However, if they are large (greater than 5cm in diameter) and if they do increase in size, then they are liable to rupture which would require an immediate emergency procedure to save the affected person’s life.
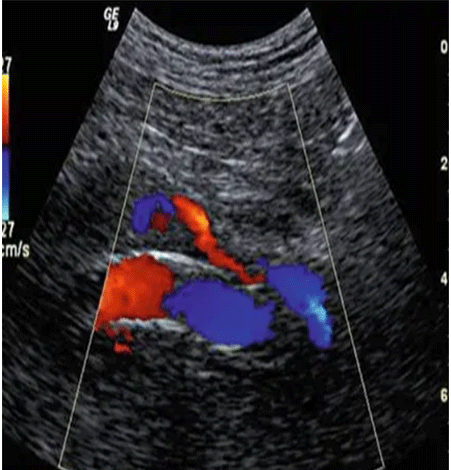
Screening for AAA is done non-invasively and painlessly through ultrasound. If someone has been diagnosed with AAA, then they are advised to get screened after every 6 months to 12 months to check whether the aneurysm is increasing in size. If it does increase in size, then accordingly to the situation, medical treatment is done.
How often should I get a screening?
If you have a family history of AAA, are aged above 50, or have had cardiovascular troubles in the past then you should get a precautionary screening every year. An ultrasound is the most cost-effective and painless option to get regular screening for AAA.
Why is early detection of AAA important?
Early detection with ultrasound will help in ruling out whether you require a surgical intervention to avoid health complications in the near future, or if a lifestyle modification like sticking to a healthy diet and incorporating physical activity will avoid the progression of the risk of a ruptured aneurysm. Early detection of AAA will prevent you from the fate of sudden death because you will be able to get medical intervention on time, to reduce the risk of complications. Physicians who deal with patients with cardiovascular disorders believe that through preventative screening through ultrasound, many lives can be saved by stopping the disease from progressing into a stage where it gets untreatable.
How can I decrease my risk for AAA?
- If you smoke then you should ask your healthcare provider to help you in following a smoke cessation plan.
- Eat a healthy and balanced diet based on low-fat foods.
- Keep your weight in a normal and healthy range.
- Try to get 150 minutes of exercise weekly.
- If you have health issues such as chronic high blood pressure or high cholesterol levels, then your healthcare provider will recommendmedications to bring the values to normal levels.
- Know about your family medical history. If someone in your family have had AAA, then that makes you at risk as well.
These are some ways that will help warn you in advance and prevent you from developing AAA. And if you have already been diagnosed with it, you may prevent its increase in size by following the above recommendations.